|
Today I spoke with a new preceptor who really sounds like a great clinician and preceptor! I thought I’d share this PMHNP’s precepting style and method.
A few details about the preceptor:
Interview with D.M, PMHNP: I see patients of all ages with all conditions. The top 5 conditions I treat are as follows:
Philosophy: I consider psychiatric care to be an art form that thrives on collaboration, interaction, and customization for each individual client. Precepting: Students will learn not only the clinical but also the business side of running a practice, including time management and CPT code selection. Medication management and psychotherapy occur with every appointment. Students sit adjacent to me as I interview clients, chart, diagnose, prescribe, and bill insurance companies. I do this mostly in person, but I can also do telepsych with students. The student reviews my charts in the morning. I give the student a brief synopsis, about a minute long, about the patient that he/she's going to see before I see the patient. I'll give the student a brief synopsis of the diagnoses, what's going on, and what medications they're on. My patients are back-to-back, and I see patients from 8:00 in the morning to 4:00 in the afternoon. I do synchronous charting, so I never take charts home. I’m done charting when I am done seeing a patient. If the student has any questions, I tell them to write them down during the patient visit. Then I will answer them either immediately after the appointment, or I will sit with the student and answer them later in the day. Also, anytime that we have a break or if a patient doesn't show up, I’ll answer questions. But I'll ask the students questions, too. I’ll ask things like, “What do you think about this? Do you have any experience with this? Why do you think I picked this medication? I really like to have that full feedback. It helps make them use their critical thinking skills. When I was a student I was with a preceptor where the students were just allowed to observe, and they didn’t provide feedback. Students just don't learn well that way. Students are just basically going off whatever their preceptor's favorite medications are, and then they adopt them as their own. And that's why I always tell people, I'm not going to give you any medication recommendations at all until I hear the full feedback. I'm going over what's going on, from sleep to anxiety to panic attacks to depression to whatever the case may be. You're not going to know all of that usually until towards the end of the interview. So I have the students do that for several encounters and usually the goal is, by the end of the rotation, that now they can do an Initial or a follow-up. Students should be able to take my notes from my last appointment and effectively do a follow-up because I write really good notes. That's one thing that I really train them to do as well. If any type of new medications or something that's kind of interesting shows up, I'll give them a little bit of homework. I might say, “Hey, teach me about X medication. That's a newer medication.” Or “Teach me about Rixalta. You don't hear that too often for bipolar patients. I give them a little useful homework. Preceptor’s choice for their EHR: So we use a system called Advanced MD EHR. It helps with practice management so I can focus on patient care. It even does marketing. It has about four tabs: 1) HPI 2) Mental Status exam 3) Patient vitals and current mood 4) Your medication recommendations, plan, and assessment. It's very user-friendly. Something that I always teach students is synchronous charting. I never bring charting home. I'm a very quick typer. I finish charting between each patient. I see a lot of patients in the day. A lot of people are going to have depression, anxiety, sleep problems. I pretty much see that across the board. So it's not good to get confused, and it's good to chart properly. That’s important. Overall, I love to teach, and I try to teach students how to do it right and do it efficiently. We think D.M., PMHNP, sounds like a fantastic preceptor and provider. We hope you found this Real World Precepting case helpful! Can you share how you like to precept? Let’s all learn from each other. (We generally don’t share names, so preceptors aren’t inundated with requests to precept!) About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on finding solutions to the preceptor shortage. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. www.PreceptorLink.com Be sure to Like, Follow and Subscribe for future NP, APRN, and Preceptor related content!
0 Comments
Time-Saving Tip for Preceptors: Empower Students as Scribes!
Hey there, fellow preceptors! I have a strategy that may help streamline your day and boost student learning. Consider having your students scribe for you! Double Duty with Scribing: Student scribes can be a fantastic asset. Here's why:
Beyond Time-Saving: Even if you already use a dictation service like FreedAI or DeepScribe, consider incorporating student scribes as well. Here's the bonus:
Let's Share the Knowledge! Student scribes can significantly enhance your day's efficiency while providing valuable learning experiences. Do you have any time-saving tips or success stories with student scribes? Share them in the comments! Let's build a supportive community of preceptors who learn from each other. About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on finding solutions to the preceptor shortage. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. www.PreceptorLink.com The PreceptorLink® Difference At PreceptorLink®, with nearly a decade of experience in preceptor matching, we go beyond simply connecting you with preceptors. We believe in QUALITY. For our NP profession to continue to have positive outcomes, we must ensure quality education. Our goal is to match quality students with quality preceptors to develop quality clinicians. Our founder, Lynn McComas, DNP, ANP-C, has leveraged her extensive experience and contacts as an NP to create our business, educate our team, and design our tech-enabled match-making App. We want to not only connect students with qualified preceptors but also equip them to make the most of this crucial learning phase. We also want to provide education to help support preceptors. If you need a preceptor, want to become a preceptor, or have a burning question about the nurse practitioner profession, we’re here to help! Lynn and The PreceptorLink® team are experts in the area of precepting and the NP profession. Check out our App, review our How It Works page, or reach out to us at 888-418-6620. www.PreceptorLink.com Be sure to Like, Follow and Subscribe for future NP, APRN, and Preceptor related content! You searched and searched, and you finally did find a preceptor! Yeah! You recently started clinicals, but now you aren’t seeing enough patients or certain types of patients that you need! If it’s not one thing, it’s another!
I frequently hear nurse practitioner students complain about this, so I wanted to share some tips on how to increase your patient census, especially if you're an NP student struggling to fill your schedule. (This approach works for new grads or clinicians who are new to a practice as well!) Understanding the Challenge Many NP students find it challenging to get enough patient hours. Sometimes, students are just not getting enough hours in general, but frequently, they are short on patients in a specific area like pediatrics or women’s health. It’s important that students have quality clinical rotations and see all ages and as many types of patients. This is especially vital since fewer physicians are going into pediatrics anymore. Not seeing a diverse population of patients can prevent you from obtaining your necessary clinical hours, hinder your learning, delay your progress, and keep you from your goals: graduation, being prepared for clinical practice, and finding a nurse practitioner job! Whether it's a low census period, such as summer, or a need for more specialized cases like pediatrics, women’s health, or geriatrics, there are effective strategies to address this issue. Below, I outline practical approaches to help ensure you meet your clinical requirements. Communicate with Your Preceptor and Office Staff So what do you do? First, communicate with your preceptor. Make sure they understand your need for more patient interactions. Frequently, your preceptor can suggest people for follow-up, but sometimes they just don’t have the time to do this in their busy day. In this case, the Office Manager or the scheduler can often help you identify potential return visits. If they are willing to take the time with you (bringing them a cup of coffee from their favorite coffee place can help incentivize them!) and review potential patients together. Look for patients who have what you need for optimal learning (and clinical check-offs. Let’s keep it real!) Patients who are due for follow-ups – blood sugar checks, failure to thrive assessments, pap smears, breast exams, imaging, or lab work. Is there a diabetic or hypertensive patient due for follow-up? Use Electronic Health Records (EHR) to identify these patients efficiently too. Another approach is to bring up a follow-up with a patient you are currently seeing. “Kelly, it’s been a few years since we did a pap smear on you. Would you like us to schedule you for follow up on that?” “Mrs. Smith, did you ever get that follow-up breast exam.” “Samantha, I see that we see your kids here as well. Do you want to schedule their sports physicals now before it gets too busy?” Build the patients you need into your schedule. This approach works when you are a new hire and you are trying to fill your schedule, too! Create Follow-Up Visits So, you’ve identified some patients. Now, what do you say when you call? (Or, if it’s the scheduler, what can they say?) I suggest something like this, “Hi, Mrs. Jones. This is Lynn McComas, and I am an NP student working with NP Smith. She wants you to come in for a follow-up on your XYZ problem. We’d love to get you in for a visit. How does this Friday work for you?” Or, “Good morning, Mrs. Jones. I’m Lynn McComas, an NP student working with NP Smith. NP Smith mentioned that you are due for a follow-up breast exam. We have an opening on Tuesday. Would that work for you? Great! Let me hand you over to the scheduler!” Suggest days when you are in the clinic, of course, but you may even need to come in on a day that you weren’t planning on coming. (Again, get the ok from your preceptor on this! They may have other students on that day.) You have now “pre-introduced” yourself to the patient, which will make the follow-up introductions even easier. A friendly reminder call can go a long way in making patients feel valued and cared for. The clinic benefits, the patient benefits, and you can get your needed hours and experience! Plus, you can study up a bit on the visit before it happens. Win, Win! Create Visits with Existing Patients Sometimes, opportunities for the required patient encounters can be created during visits with existing patients.
Leveraging Technology Utilize patient portals to identify patients who are overdue for visits, labs, or imaging for easy scheduling and for automated reminders. These tools can significantly reduce no-show rates and keep your schedule full. Then, for best results, follow up with a phone call. Expanding Your Network to Other Providers Network with other healthcare providers in the practice or hospital. This can be especially helpful for Acute Care or inpatient settings, but really for any sites that have multiple providers. Let them know your needs and ask if you can see any [peds, women’s health, cardiac, etc.] patients with them. (Once again, be sure to get your preceptor’s permission for this first.) This not only helps you see the patients you need, but it also helps you meet other providers (for future clinicals or general networking). Conclusion Finding the types of patients that you need for clinical rotations can be challenging, but with proactive strategies and a positive attitude, you can turn this around. Communicate with your preceptor, take initiative, and utilize available resources to maximize your clinical experience. These strategies, grounded in practical experience, can make a substantial difference in achieving your clinical rotation goals. Remember, every challenge is an opportunity to learn and grow. Keep pushing forward, stay patient, and continue to build your skills. Keep on learning! About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on finding solutions to the preceptor shortage. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. www.PreceptorLink.com Be sure to Like, Follow and Subscribe for future NP, APRN, and Preceptor related content! Embarking on your clinical rotations can be both exciting and nerve-racking. To help ensure your success, it's crucial to be prepared. According to our preceptors, here are 13 essential questions to ask before you start your clinicals. Knowing the answers to these can help you prep for success!
1. Is there someone who can orient me, and if so, who will that be? Understanding whether there will be an orientation and who will be responsible if there is one is useful. This person will help you get acquainted with the clinical environment and the expectations. The person orienting you might be the preceptor, a medical assistant, or another student. In some cases, there is no one, and you may just have to jump in and figure things out yourself. It’s great to know this information ahead of time! 2. Will I be able to shadow you, and if so, for how long? Determine the duration and extent of shadowing. This varies based on the student’s experience level and the preceptor’s preference. Clarify this to ensure you’re on the same page. Some preceptors might expect you to jump right in, while others may have a structured shadowing period. 3. Can you describe how you typically precept nurse practitioner students? Understanding the preceptor’s approach is essential. Will you start by shadowing, then conducting patient histories, followed by joint exams and planning with the preceptor? This is a fairly typical approach, but it can really vary from preceptor to preceptor. Especially if you have someone who's never precepted, they might think that you're more prepared than you are. Or, the opposite may be true. Perhaps you've been doing clinicals for a while, and you're ready for more independence, but your preceptor is thinking all you're going to do is shadow. Try to have a conversation and clarify things. 4. What is the typical length of patient visits, and how many patients are seen daily? Know the patient flow to manage your time effectively. You might need to see a specific number of patients per day to meet your program’s requirements. You might need to explain that you need to see at least eight patients a day or one per hour. It all depends on what your requirements are and what the preceptor will allow. 5. Charting: Know what’s expected of students Will you be allowed to chart? It is legal at a Federal level as long as certain protocols are followed, but is it allowed at the site? What is the preferred approach to charting? Will you do mock charting? If the student is allowed to use the EHR, will you receive any kind of EHR training? Electronic Health Record (EHR) systems can vary. Inquire about training and consider doing some preparatory research or watching tutorial videos. 6. Who informs patients an NP student is working with the preceptor? Understand who will notify patients about your involvement in their care. Whether it’s the front office staff, the medical assistant, the preceptor, or yourself, knowing this process is important for a smooth introduction. Occasionally, the student might just pop in and say, “Hi. I’m a nurse practitioner student who’s working with Dr. Smith today. If it’s ok with you, I’ll be starting our visit. Then, Dr. Smith will be in, and we’ll finish together. Would you be comfortable with that?” Someone should ask the patient’s permission, but there are ways to do this and receive a willing response. If you sense hesitation, reassure the patient that it’s ok if they prefer not to have a student during the visit. We need to respect the patient’s wishes. 7. Is there a particular way that you want me to “report” the patient to you? Everyone is different, and it's helpful if you can get a quick explanation of your preceptor’s presentation style preference. (Check out our Resources Page for the Video Vignettes on Precepting link to the NONPF page.) 8. What are the preceptor’s expectations regarding your schedule and attendance? Clarify the preceptor’s schedule expectations. Be prepared to match the preceptor’s hours and avoid frequent absences or early departures. Communicate any necessary schedule changes in advance, but respect the preceptor’s requirements. Students really need to plan their schedules and lives. Here are some frequent complaints we hear from preceptors:
9. Have you precepted a nurse practitioner student before? This question helps gauge the preceptor’s experience with NP students and may influence their teaching style and expectations. If they have only precepted med students or therapy students, there may be a different level of expectation. 10. What is the dress code, and what should I bring? Confirm the required attire and necessary items such as scrubs, lab coats, name tags, lunch, books, apps, a computer, and a notebook. 11. Where should I park? Find out about parking arrangements, including any associated costs and specific locations. 12. What are the most common diagnoses in this practice? I always recommend that you ask the 10 to 20 most common diagnoses that you'll be seeing in the practice. Then, study those so that you know how to take a good history, write a good SOAP note, make an appropriate plan, and know the most commonly used drugs and associated therapeutics for the conditions seen. 13. Is there anything else I should know? This open-ended question can reveal additional expectations or information that can help you better prepare. (Also, check out our Resources Page for the Video Vignettes on Precepting link to the NONPF page.) Preparation is key, so take the initiative and clarify these points with your preceptor. If you think of other important questions, feel free to share them with us. This is "Real-World Precepting"—practical, honest, and designed to set you up for success. Keep on learning and prep for success! About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on finding solutions to the preceptor shortage. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. Part of the “Real World Precepting Series”  Precepting via telepsych is a transformative approach in psychiatric education, offering numerous advantages over traditional in-person methods. One of the standout benefits is the ability to precept multiple students simultaneously, enhancing the learning experience and optimizing the preceptor's time. Additionally, if it’s allowed by schools, one preceptor can precept multiple students at the same time. Let me share the story of one of our beloved preceptors, KP, who exemplifies the effectiveness of telepsych precepting. Meet KP: A Model Telepsych Preceptor KP is an experienced PMHNP. She owns her own practice and manages both patient care and student precepting entirely through telepsych. Students log in from home on a HIPAA-compliant platform. This method has proven to be highly effective, with students expressing immense satisfaction with their learning experiences under her guidance. Students enjoy the flexibility and enjoy learning from other students in a group-like environment. KP treats a diverse range of patients across the age spectrum, making her practice a rich learning environment. KP typically sees between 8 to 15 patients a day. She is able to precept two to four students at the same time, thanks to the flexibility and efficiency of telepsych. Telepsych allows her to accommodate even more learners, maximizing the educational opportunities for everyone. The Technology Behind Telepsych Precepting KP utilizes a platform called Tebra (formerly known as Kareo), which she praises for its simplicity and efficiency. The platform provides a one-click video link that students can easily log into, facilitating seamless integration into patient visits. KP rates this platform highly, giving it a solid 9 out of 10, based on her extensive experience. KP’s feedback on this platform is unsolicited and purely based on her experience. (PreceptorLink® does not receive anything for recommending the platform, nor do we have personal experience using it. You are encouraged to review different telepsych platforms if you are considering adding telepsych/telepsych precepting to your practice.) KP’s Precepting Approach The precepting process begins with patients giving consent for students to be present during their visits. Once consent is obtained, students can observe and participate in the consultation. Initially, KP leads the sessions, allowing students to ask questions and interact after the visit. As students become more confident and knowledgeable, she gradually allows them to take a more active role, including leading the patient interaction under her supervision. A key element of KP’s teaching style is her use of quizzes on medications and therapeutic approaches post-visit. This method encourages critical thinking and ensures that students are well-prepared for real-world practice. For instance, she might ask questions like, "Why do you think I chose this medication over another?" or "What additional therapeutic approaches could be considered for this patient?" These questions not only reinforce learning but also stimulate deeper clinical reasoning. The Impact of Effective Telepsych Precepting KP's dedication to her students is evident in her interactive and challenging teaching methods. Her approach ensures that students are not only knowledgeable but also capable of applying their knowledge in practical settings. She is highly regarded by her patients, students, and the team at PreceptorLink®, illustrating the profound impact a skilled preceptor can have. She has our highest marks as a preceptor. Embracing Telepsych Precepting in Your Practice Telepsych precepting is a valuable tool for modern psychiatric education. It offers flexibility, efficiency, and the ability to provide high-quality training to multiple students simultaneously. Some clinicians offer only in-office telepsych, where the student is present with the preceptor and/or preceptor’s office. This option, while still valuable to learn, reduces the number of students who can benefit from the opportunity unless they have an available conference room or room where multiple students can sit. By incorporating telepsych into your precepting practices, you can contribute to the development of future psychiatric professionals while maintaining patient care standards. We hope this insight into telepsych precepting is helpful and inspires you to explore its benefits. By embracing this innovative approach, you can enhance your teaching practice and support the next generation of psychiatric clinicians. Keep on learning! Check out our video on this same topic on YouTube! Like, Subscribe, and Share for great precepting and NP/APRN-related content! The PreceptorLink® Difference
At PreceptorLink®, with nearly a decade of experience in preceptor matching, we go beyond simply connecting you with preceptors. We believe in QUALITY. For our NP profession to continue to have positive outcomes, we must ensure quality education. Our goal is to match quality students with quality preceptors to develop quality clinicians. Our founder, Lynn McComas, DNP, ANP-C, has leveraged her extensive experience and contacts as an NP to create our business, educate our team, and design our tech-enabled match-making App. We want to not only connect students with qualified preceptors but also equip them to make the most of this crucial learning phase. We also quant to provide education to help support preceptors. If you need a preceptor, want to become a preceptor, or have a burning question about the nurse practitioner profession, we’re here to help! Lynn and The PreceptorLink® team are experts in the area of precepting and the NP profession. Check out our App, review our How It Works page, or reach out to us at 888-418-6620. www.PreceptorLink.com About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on finding solutions to the preceptor shortage. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. So, you have finally said yes to a student who needs a PMHNP preceptor! (Or you’re at least considering it.) Great! Thank you! Providing quality education to these future mental health providers is vital, and there is a great need for more mental health providers. But, precepting a PMHNP student is very different than precepting a Family Practice student. So, now you are asking, “How do I precept a PMHNP student?” Whether you are a psychiatrist, a PMHNP, or a therapist, here are some important things to consider first if you are going to precept a PMHNP student:
1. Patient Permission:
2. Decide how you will precept.
3. Will students be able to see the patients and visa versa?
4. Will students be able to participate in the visit?
Those are some of the things you will want to consider when you precept a PMHNP student. You’ll find some video vignettes on precepting in general from NONPF, in case you want to check that out, too. This is a great article that goes into the topic in more detail as well. We’ll talk about more specifics on precepting the PMHNP student in future blogs, so make sure to follow PreceptorLink®! And hopefully, you’ll be a PreceptorLink® preceptor! Thank you for precepting! We’re happy to advise you if you ever need it. We have decades of experience when it comes to precepting NP students! Just email or call us at [email protected] or 760-604-0913 About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on finding solutions to the preceptor shortage. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. www.PreceptorLink.com Med management is not the only component of the Psych Mental Health Nurse Practitioner (PMHNP) student’s education. Learning how to develop a therapeutic relationship with patients is also a vital part of their education. And who better to help teach this to a PMHNP student than a seasoned clinical therapist? A quality therapist can contribute to a well-rounded clinical experience for PMHNP students. However, finding a therapy preceptor for a PMHNP student can be incredibly challenging.
I do frequently hear from therapists who want to precept Nurse Practitioner (NP) students, but administrative hurdles can stand in the way. Many times, Administrators don’t understand some of the benefits of allowing a therapist to precept a PMHNP student. So, what you can say to your boss or Administration to showcase the benefits of precepting and encourage them to say yes? And what can a PMHNP student say to a therapist to help convince him or her to precept them? (Share this article with a potential therapist!) Here are some ideas: Collaboration and Improved Care:
Building a Pipeline of Potential Hires:
Investing in the Future:
Utilizing Your Expertise:
Mutual Learning and Growth:
Show Initiative and Be Flexible:
Highlight Your Enthusiasm:
By framing precepting as an investment in the practice, the future of mental healthcare, and your professional development, you can convince your boss to give it the green light. Remember, your enthusiasm for precepting will be contagious. About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on finding solutions to the preceptor shortage. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. www.PreceptorLink.com If you precept long enough, there is a good chance you will have an NP student who needs to be counseled or have their behavior addressed. Handling difficulties with a student during a clinical rotation can be challenging, but it's important to know how to handle the situation if it occurs. It’s essential for the preceptor to approach the situation professionally, constructively, and with the best interests of the preceptor, student, patients, and institution in mind. Before we get into the details, one thing I’ve heard from students several times before is that they had no idea there were issues or that the issues were that significant. So, whether this was something that was not understood by the student, not taken seriously by the student, or never clearly addressed with the student, following these steps will help avoid any confusion. Here are steps and best practices for preceptors facing such issues: 1. Self-Assessment and Documentation: Before taking any steps, assess your feelings and perceptions. Make sure your concerns are based on objective observations and not personal biases. Document specific incidents or areas of concern in detail. This can help the student understand your exact concerns. This documentation can also be crucial in case other parties need to be involved. 2. Private Discussion with the Student: Initiate a private, one-on-one conversation with the student. The key here is to be: - Clear and Specific: Outline your observed behaviors or performance issues. - Constructive: Instead of just pointing out problems, suggest ways for the student to improve. - Empathetic: Understand that students can have off days, and external pressures can affect performance. Listen to their side of the story. - Non-confrontational: Use "I" statements instead of "you" statements to reduce defensiveness. For instance, "I noticed that…" instead of "You always…". 3. Set Clear Expectations and Develop an Action Plan: Together with the student, create a plan to address the areas of concern: - Goals: What should the student achieve by the end of the rotation? (Or end of week or month) - Steps: How can they achieve these goals? - Timeline: By when should they achieve each step? - Feedback sessions: Regularly scheduled check-ins to evaluate progress. Determine how often the feedback should occur and follow up accordingly. 4. Ongoing Feedback: Regular feedback is crucial. Praise improvements and address new or continuing issues promptly. This helps the student understand that you're not just focused on their weaknesses but also appreciate their strengths. 5. Involve Faculty if Necessary: If the problems persist despite your interventions, or if there are serious concerns about patient safety or professional behavior, it might be time to involve the student's academic faculty. - Communication: Ensure you communicate your concerns clearly and provide your documentation. - Collaboration: Work collaboratively with the faculty to decide on the next steps. They might provide additional resources, recommend remedial work, or suggest other interventions. Precepting a challenging student can be difficult. Fortunately, this is not a frequent occurrence! But if you need it, there are also links on our Resources page with videos on Precepting the Challenging Student. While I hope that things do not escalate, there are times when the student needs to be removed or dismissed from the clinical rotation. We’ll discuss that challenging topic in an upcoming issue. We’ll also discuss things from the student’s perspective on Managing Preceptor Problems in Student Clinicals because they can happen on both sides! Stay tuned. In the meantime, keep on learning, and thanks for precepting! About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on solutions to this problem. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. As a seasoned Nurse Practitioner (NP), I understand the vital role collaboration plays in mental healthcare. Therapist involvement in the education of Psych Mental Health Nurse Practitioner (PMHNP) students is a prime example of such collaboration.
Many PMHNP programs require students to complete therapy rotations in addition to rotations that focus more on medication management. These programs actively seek “therapy preceptors.” These are licensed, masters-prepared, or higher therapists who act as preceptors—essentially, short-term mentors—for their students. Just as you, the therapist, once relied on a supervisor clinician, these students require guidance into the world of psychotherapy in their program. Here's why partnering with a PMHNP student as a therapist is a mutually beneficial experience:
It's crucial to remember that PMHNP students are not observing therapy sessions to learn how to become therapists themselves. Their focus is on understanding the therapist's role in the patient's overall care plan. This may involve observing in-person or virtual sessions, learning how therapists develop rapport, conduct assessments, and collaborate with PMHNPs on treatment approaches. By partnering with a PMHNP student, you're not only contributing to their education but also fostering a collaborative healthcare environment that ultimately benefits the patients you both serve. Consider becoming a psych NP preceptor or a nurse practitioner student preceptor today. About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. Determined to make a difference in “the Preceptor Problem,” Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University, where she focused on solutions to this problem. She is the owner and founder of PreceptorLink®. The company’s goal is to simplify and streamline the process of preceptor matching while maintaining quality and professionalism throughout. www.PreceptorLink.com Why is PreceptorLink® the best preceptor-matching company?
It’s The “PreceptorLink® difference.” - Experienced, nurse practitioner-led team - Fast placement- most within 1-3 days - Unmatched expertise - Extensive preceptor network - Proven success rate - Dedicated support. We complete paperwork for students and preceptors - Quality - Our goal is to provide quality clinical education Lynn McComas, DNP, ANP-C, is the founder and owner of PreceptorLink®, is dedicated to students and preceptors, and is actively involved in the business. She is a seasoned NP who knows and cares about the profession...because this is her profession! She is actively working with nursing organizing bodies, schools and faculty, and decision-makers in the profession. Her doctoral studies at Duke focused on finding solutions to the preceptor problem for NPs. She continued her studies with a focus on business through the Goldman Sachs Small Business program. As an NP-entrepreneur, Lynn understands the business and clinical sides of this issue. The PreceptorLink®️ team are your experts in preceptor matching for APRNs and NPs. PreceptorLink® has been matching NP preceptors since 2014, so we have the experience, connections, and know-how to get the job done. We are here for the long haul because we want to work toward positive change in the profession. Contact PreceptorLink today! So, you've set your sights on becoming an Acute Care Nurse Practitioner (ACNP), and now you need to make the important school choice. Good for you for looking at your options. It’s a very important question. Here’s your critical next step: Picking the right program/school. Let's face it. There are hundreds of options out there, and it can feel like wandering through a clinical labyrinth. But fear not fellow future NP colleges! I'm here to equip you with the map and compass you need to make an informed decision.
First things first: Consider your "must-haves." What learning format suits your lifestyle? Do you crave the camaraderie of on-campus classes, or does online flexibility better fit your busy schedule? Does the program offer your preferred specialty, like cardiology or neurology? Remember, this is an investment in your future, so choose a program that aligns with your aspirations and learning style. Here are some key areas to investigate: Clinical Placements: This is where the rubber meets the road. ACNP programs must provide supervised clinical placements in actual acute care settings, not just clinics or outpatient facilities. Remember, you're training to manage critically ill patients in fast-paced environments. Dig deeper:
Faculty Credentials and Support: Your professors play a crucial role in shaping your ACNP expertise. Make sure they hold current clinical practice experience and possess relevant specializations. A faculty deeply ingrained in the acute care world can offer invaluable guidance and share real-world scenarios. And make sure you will have access to faculty. Support services, such as academic advising, tutoring, and career counseling, are essential components of a supportive educational environment. Curriculum: The curriculum should serve as a detailed map, guiding students beyond theory to the practical skills necessary for the acute care setting. A well-rounded curriculum encompasses pathophys, pharm, and health assessment, and it integrates specialized courses focusing on acute and critical care management. Personally, I love programs that include in-person hands-on actually held at the educational institution. These are often referred to as OSCEs, which stands for “Objective Structured Clinical Examination.” OSCEs may require a trip to your university, but it's a great way to practice and demonstrate your clinical skills in a standardized, safe, clinical scenario. Embrace and welcome this opportunity! Accreditation: This might seem obvious, but accreditation by a recognized organization like the Commission on Collegiate Nursing Education (CCNE) or the Accreditation Commission for Education in Nursing (ACEN) ensures your program meets rigorous quality standards. Don't settle for anything less – your future career and patient safety depend on it. Financial Aid and Scholarship Opportunities: Let's be honest, these programs aren't cheap. Explore financial aid options, scholarships, and loan programs offered by the institution and external organizations. If you are in the military, check out how that might benefit you. Remember, investing in your education is investing in your future earning potential. Beyond the checklist: Consider the program's culture and values. Do they resonate with your own? Look for a supportive environment that fosters collaboration, critical thinking, and a commitment to evidence-based practice. Don't underestimate the power of feeling comfortable and valued during your educational journey. Outcomes: A Measure of Success Finally, program outcomes, such as graduation rates, board certification pass rates through ACCN, and employment statistics, offer a lens through which to gauge the program’s effectiveness. High pass rates and strong employment outcomes can indicate a program’s success in preparing students for the real-world demands of the acute care setting. A message from our preceptors: At PreceptorLink®, we help place Acute Care NP students every day. One complaint we regularly hear from ACNP preceptors is that Acute Care Nurse Practitioner students do much better if they have experience in an acute care setting like an ICU or critical care unit. They report that the students who really struggle are the ones who don’t have this background. While not every school requires ICU experience as entry criteria, our preceptors strongly advise at least 2+ years in a true critical care ICU setting. This will also help you know whether this is your passion! Good advice all the way around. Remember, choosing your ACNP program is a personal decision. Take your time, research thoroughly, and ask all the questions. Trust your gut and choose wisely, and you'll find the program that prepares you to excel in the dynamic world of acute care. Now go forth, conquer that educational maze, and emerge a confident, compassionate ACNP ready to make a real difference in the lives of critically ill patients! Also, as a fellow NP, I understand the excitement and challenges you face. Feel free to reach out if you have any further questions--I'm here to support you every step of the way! About the Author: Lynn McComas, DNP, ANP-C, is an experienced nurse practitioner and an expert on the topic of precepting. She has held many leadership positions in nurse practitioner organizations. It was while attending her local CANP chapter meetings that she frequently witnessed students begging for preceptors, and she thought, “If we paid preceptors, I’ll bet more would be willing!” That is how the concept of PreceptorLink® was born. Determined to make a difference in “the Preceptor Problem, Lynn went on to obtain her Doctorate in Nursing Practice (DNP) at the esteemed Duke University. At Duke, every assignment, including her final Capstone, was on finding solutions to the preceptor problem. Her final project was the development of “The Preceptor Playbook: A Checklist and Templates for Precepting Nurse Practitioner Students.” Lynn has presented and done poster presentations at AANP and other conferences on the subject of precepting and finding Solutions to the Preceptor Problem for NPs. By Lynn McComas, DNP, ANP-C NP and APRN students, did you know that you can use a Compact State License (CSL) to help you find a preceptor? A compact nursing state refers to the Nursing Licensure Compact (NLC). Basically, it allows license reciprocity for RNs and LPNs to practice in other compact states. For NP, APRN, and RN students, this can open up options for other states where they can do clinicals. You do have to apply to get a CSL in most states, although some states do it automatically, so check with your state’s Board of Nursing (BON) for specific requirements. Check out the NLC website to see the most recent map. Here is a picture of the most recent Compact State Licenses, effective March 25, 2024.
So, if you are an NP student, check it out. Maybe it’s the perfect time to stay with a friend, a relative, or even an Airbnb just so you can get that clinical rotation done! We’re sorry it’s so hard for students, but this may open up another channel for you to find a preceptor. Keep on learning, everyone!
The PreceptorLink® Difference At PreceptorLink®, with nearly a decade of experience in preceptor matching, we go beyond simply connecting you with preceptors. We believe in QUALITY. For our NP profession to continue to have positive outcomes, we must ensure quality education. Our goal is to match quality students with quality preceptors to develop quality clinicians. Our founder, Lynn McComas, DNP, ANP-C, has leveraged her extensive experience and contacts as an NP to create our business, educate our team, and design our tech-enabled match-making App. We want to not only connect students with qualified preceptors but also equip them to make the most of this crucial learning phase. We also quant to provide education to help support preceptors. If you need a preceptor, want to become a preceptor, or have a burning question about the nurse practitioner profession, we’re here to help! Lynn and The PreceptorLink® team are experts in the area of precepting and the NP profession. Check out our App, review our How It Works page, or reach out to us at 888-418-6620. www.PreceptorLink.com By Lynn McComas, DNP, ANP-C As a longtime nurse practitioner, I frequently hear the question: “Should I become a PMHNP or an FNP? I just don’t know.” Yes, a psych mental health nurse practitioner (PMHNP) versus a family nurse practitioner (FNP). Both are great professions, but very different. So, let's talk about some of those differences.
Becoming a Provider: A Big Step First and foremost, consider whether becoming a provider is the right fit for you. Transitioning from registered nurse (RN) to provider is a significant shift with increased responsibility. You'll be directing care and making diagnoses. Self-reflection is crucial to ensure this path aligns with your aspirations, abilities, and your personality. Once you’re certain that being a PROVIDER is a good fit, then let's move on! ✅ Matching Your Passion to Your Path As you likely know, an FNP can prescribe some psych medications, but if Psych really is your thing ✅, if you love Psych ✅, if those are “your people” ✅, I would encourage you to get your PMHNP. On the other hand, if psych isn’t really your thing, if you're more of a generalist, and you like the idea of seeing a variety of things and taking care of a lot of different kinds of patients, a little bit of everything, then perhaps being an FNP is a better fit. PMHNP Preceptor Experience: Varied Opinions Do you need experience as a psych RN to become a PMHNP? While I've heard preceptors give different responses to this question, most recommend that you have psych experience either as an RN or in a related field. This will help ensure that you know this population really is who you want to spend your career caring for. But just the other day, I spoke with a PMHNP who said she preferred students with no psych experience so she could “shape them.” However, the majority of our preceptors recommend having some professional psych experience. FNPs Working in Psych: Yes or No? What about being an FNP and working in Psych? Yes, as an FNP, you can prescribe psych medications, and in primary care, you will likely prescribe some psych meds. But we do want to try to stay within our scope of practice. If you really love psych, become a PMHNP. Many of our FNP preceptors have decided to become dual certified as both an FNP and PMHNP. Diverse Work Environments for PMHNPs PMHNPs work in both inpatient and outpatient settings. Inpatient settings can include locked psychiatric facilities, skilled nursing facilities, correctional institutions, and residential treatment programs. Outpatient settings encompass mental health services in clinical settings. Patients often transition between these settings during their care journey. The Rise of Telepsych One positive outcome of the COVID-19 pandemic is the widespread adoption of telepsych, offering flexibility for both providers and patients. Many PMHNPs are leveraging telepsych and obtaining licenses in multiple states to expand their reach. This trend may present exciting opportunities for PMHNPs, with some even starting their own practices, particularly in Full Practice Authority (FPA) states. We’ll talk a lot more about the Considerations and Implications of Telepscych for PMHNPs in future articles. Watch our blog for updates! FNP Work Settings and Specialties FNPs typically work in outpatient settings, such as primary care, internal medicine, geriatric medicine, and urgent care. However, they can also venture into specialty areas like cardiology, sleep medicine, endocrinology, integrative medicine, or neurology, often pursuing additional training. Some FNPs work in emergency rooms, frequently after obtaining additional Emergency Nurse Practitioner (ENP) certification. There are many different things FNPs can do, but those are some of the most common settings. Compensation Considerations While nurse practitioners generally earn competitive salaries, the exact amount varies depending on location and demand. To date (2024), PMHNPs typically command slightly higher salaries than FNPs, but salary shouldn't be the sole deciding factor. Additionally, I am hearing from our PMHNP colleagues that salaries are starting to flatten as the field becomes more saturated. Research potential job markets to avoid entering oversaturated areas. Additionally, a review of the many NP Facebook pages will reveal that some NPs have returned to working as RNs again. Whether the reason is a lack of job opportunities, burnout as a provider, a preference for bedside nursing, or something else, it’s a disturbing trend. Making an Informed Decision Ultimately, the choice between PMHNP and FNP hinges on many factors, including your passion, preferred patient population, and desired work environment. I wish you the very best in your decision to become a nurse practitioner. Keep on learning! By Lynn McComas, DNP, ANP-C The PreceptorLink® Difference At PreceptorLink®, with nearly a decade of experience in preceptor matching, we go beyond simply connecting you with preceptors. We believe in QUALITY. For our NP profession to continue to have positive outcomes, we must ensure quality education. Our goal is to match quality students with quality preceptors to develop quality clinicians. Our founder, Lynn McComas, DNP, ANP-C, has leveraged her extensive experience and contacts as an NP to create our business, educate our team, and design our tech-enabled match-making App. We want to not only connect students with qualified preceptors but also equip them to make the most of this crucial learning phase. We also quant to provide education to help support preceptors. If you need a preceptor, want to become a preceptor, or have a burning question about the nurse practitioner profession, we’re here to help! Lynn and The PreceptorLink® team are experts in the area of precepting and the NP profession. Check out our App, review our How It Works page, or reach out to us at 888-418-6620. www.PreceptorLink.com So, Why Don’t Providers Want to Precept?
I often see students on Facebook and similar forums say that they don’t understand why providers won’t precept. These same students also often promise that they will precept one day for free. That is a completely understandable perspective after all these poor students have been through in their preceptor searches! So, why are providers often hesitant to precept? Here are several of the reasons why: 1. Time Constraints: Precepting can require a significant time commitment. Providers have busy schedules, and adding the responsibility of mentoring students can be challenging. They need to balance patient care with teaching, which can extend their work hours. And that can also affect their bottom line. 2. Lack of Adequate Compensation and Incentives: In many cases, precepting doesn't come with financial incentives, recognition, or compensation. Providers may feel that the extra effort and time devoted to precepting are not adequately rewarded and just plain not worth it. 3. Increased Responsibility and Liability: Precepting involves overseeing the clinical work of students, which adds an extra layer of responsibility and potential liability. Providers or management might be concerned about the quality of care provided to patients under their supervision and the legal implications of precepting. 4. Insufficient Training or Confidence in Teaching Skills: Some providers may feel they lack the necessary skills or training to effectively mentor students. This can include uncertainty about how to evaluate students, provide constructive feedback, or manage different learning styles. 5. Administrative Burden: Precepting can involve additional administrative tasks such as completing agreements, performing evaluations, coordinating with educational institutions, and managing scheduling. This added workload can be a deterrent. 6. Impact on Patient Care and Workflow: Providers might be concerned about the potential impact on patient care and clinic workflow. Students often require more time per patient, which can lead to longer wait times and reduced efficiency. 7. Personal Preference: Some providers may simply prefer to focus solely on patient care without the added role of an educator. And, let’s be honest, not everyone should be a preceptor. Sometimes, it’s just not that individual’s skill set. (Although Preceptor Education may help that!) 8. Workload and burnout: Healthcare providers may already be dealing with heavy workloads and burnout due to the demands of their clinical practice. Taking on additional responsibilities, such as precepting, may further add to their workload and stress levels. 9. Lack of support from Management: Frequently, even though the preceptor is willing to precept, management says no. This is extremely unfortunate and frustrating to encounter, but it is their bottom line. Whether you are a healthcare professional or a healthcare institution, we must all work together to address the concerns and disincentives to precept. Providing adequate support, training, compensation, and recognition for preceptors could encourage more providers to take on this vital role. And, students, we do hope you will precept when you are on the “other side!” Whether you are a new grad or a seasoned NP, don’t forget to ask about precepting during job negotiations. You don’t want to be surprised down the road by policies you didn’t know about. We must advocate to educate the next generation of NPs! Yep! That question again. Once again, this question is popping up in articles and forums, and there’s a pretty obvious consensus developing about the reasons why nurses may be leaving the nursing profession.
The fact is this is not the first time we’ve seen a nursing shortage or seen a nursing exodus. As a longtime nurse and even longer time nurse practitioner, I’ve sure seen it before. Any experienced nurse witnessed them in the 70’s, 80’s and early 90’s. But the shortage was always filled with a fresh supply of nursing school graduates. So, what makes things feel a little different this time around? Nurses Are Burned Out: It’s no real secret, nursing is a physically and emotionally demanding job, with long hours, staffing shortages, high workload and stress levels, and exposure to traumatic situations all just part of the daily ‘normal’. Many experience anxiety or depression because of the job-related stressors. Although 2021 was a peak year, and the numbers have improved slightly, the exhaustion, cynicism, and detachment of burnout can be a career ender, for even the most dedicated of nurses. Nurses Feel Undervalued: If nothing else, the Covid Pandemic served to prove something that many nurses had been suspecting for a long time: our government, our employers, and the communities we dedicate our lives to are often long on talk and short on action when it comes to supporting the needs and aspirations of the nursing workforce. Hospital needs to cut costs? Invariably, efficiency consultants or projects look to cutting nursing staff as the answer. (I think they need to be a patient and feel the outcome of THAT decision!) The chronic lack of support, recognition, and career advancement opportunities, as well as the crushing workload that’s become average across the profession, sends far too many good nurses out looking for greener pastures elsewhere. Nurses’ Work Environments Are Often Toxic Why is it that nursing is especially prone to bullying? Bullying and harassment from colleagues and supervisors, inadequate staffing leading to unsustainable hours and responsibility loads, and a culture that downplays a nurse’s mental health and encourages a “suck it up” mentality. All of these issues and more create a work environment that nurses are leaving in droves, in order to find a healthier work-life balance. Nurses Are Getting Older And Ready To Retire As the workforce ages, a perfectly normal part of any profession, nurses simply retire. The trouble arises as we begin to see enrollment in nursing programs trend downward while nurses from the Boomer generation begin to retire at higher and higher rates every year. This resulting loss of a skilled and knowledgeable nursing workforce may result in higher turnover rates, and a shrinking pool of experienced nurses to train and mentor the new generation. The Nursing Profession Is Less Attractive Because of all these issues, we are starting to see a shift in the trends of young people entering healthcare careers, as well as established nurses leaving the profession to pursue other opportunities. Nursing is a versatile profession with many specialties and options for career advancement, but without support and encouragement, nurses are choosing to transition to different roles within or outside of healthcare or pursue further education and training in a different field altogether. It’s important to remember that simply identifying why nurses are quitting is just a small part of solving the problem. The real question we must answer as an industry is, what can we do to encourage nurses to STAY? Instead of wringing our hands over all the problems, let’s begin to address these issues through policy and cultural shifts. Let’s begin to promote a positive work environment by addressing nurses' mental health seriously. Let’s promote and prioritize a health work-life balance for nurses. Let’s court the younger workforce with career advancement opportunities and other benefits. In general, let’s focus the resources of the healthcare industry on making nursing a healthy, thriving profession that our best and brightest are attracted to. Let’s stop thinking of nurses as commodities. Nurses are highly educated professionals who need to be valued and respected. A change in this philosophy will help fill nursing schools and nursing positions. Each of these questions is meant to ask potential NP students to think deeply about the factors that are most important in their educational and professional journey.
Choosing the right specialty for your Nurse Practitioner (NP) career is critical, both for your long-term job satisfaction and for your success in the job market after graduation. Finding the balance between an area that suits your skills, interests, lifestyle, and personality and one where you can actually successfully land a job takes a lot of consideration and research. It’s a decision that you must take seriously, and there is much to consider. Here are a few thoughts to help you through the decision-making process:
Once you’ve answered those questions, it’s time to do some research. You can comb through LinkedIn and other job board postings, talk to mentors in the field, and reach out to current practitioners in your area to find out more about their experiences. Facebook groups for NPs can be a great way to connect with experienced practitioners and learn a little bit about their stories. Although this can be hard in today’s healthcare environment, see if you can shadow NPs in different specialties to get a firsthand experience of their day-to-day work. This can help you better understand the nature of their practice, patient interactions, and job responsibilities. It can also help you determine if a particular specialty is the right fit for you. What you’re looking for is that “sweet spot” where location, job market, and your healthcare passions all intersect. This extra effort in the short run, before you commit to a program of study, can save you a lot of trouble and disappointment in the long run! Who doesn’t want to earn a little extra income while still putting your Nurse Practitioner (NP) or Physician Assistant (PA) skills to good use? If that’s you, you're in the right place! We've got a list of intriguing side hustles tailored for NPs and PAs and PAs that not only let you do what you know and love but also pad your wallet a bit. Let's dive into the possibilities! I’d always recommend that you “stay in your lane” and not fake your area of expertise, however. 1. Home Healthcare Assessments: Conduct home healthcare assessments part-time, helping patients with chronic conditions manage their health in the comfort of their homes. I did this and loved it. A love of seniors and reliable care are beneficial. I had to drive a lot, and you need to make sure that they allot you enough time for the visits AND drive time. Try to make sure you are in one drivable area. This can also be a great job if you only want a part-time job with some flexibility. 2. Online Health Coaching: Offer part-time virtual health coaching services to individuals seeking guidance on nutrition, fitness, and overall well-being. This can be done via video calls or chat platforms. Health coaching is very popular these days, and there are even health coaches for specific medical diagnoses, like Diabetes, Arthritis, Cancer, etc., so you can specialize in what you know! There are also Health Coach Certifications that you pay for. 3. Freelance Medical Writing: Sharing Expertise through Words As NPs and PAs, we possess a wealth of medical knowledge, which can benefit a wider audience through the art of writing. Freelance medical writing allows clinicians to educate and inform through articles, blog posts, and e-books. This side hustle not only offers a creative outlet but also contributes to the dissemination of valuable healthcare information. 4. Medical Consulting: Shaping the Future of Healthcare Do you have a penchant for problem-solving and innovation? You might venture into medical consulting. This role involves providing strategic guidance to healthcare organizations, startups, or clinics. NPs and PAs' clinical experience and insight can help shape the future of healthcare delivery and management. Try using LinkedIn to reach out to those who might need your services, and, of course, make sure your LinkedIn profile and resume support your skillset. 5. Health and Wellness Blogging: Consider starting a health and wellness blog where you share your expertise on staying healthy and balanced in life. You can monetize your blog through ads, affiliate marketing, or sponsored content. 6. Educator for Certification Prep: Leverage your knowledge to teach and prepare aspiring nurses or NPs and PAs for certification exams. Create online courses or offer one-on-one tutoring sessions. Many NPs (like the amazing Margaret Fitzgerald, DNP, FNP-BC, FAANP, and Amelie Hollier, DNP, FNP-BC, FAANP) have started or moved into this space (like Sarah Michelle, FNP). 7. Health-related YouTube Channel: Start a YouTube channel where you discuss health topics, provide advice, and share tips on maintaining a healthy lifestyle. Monetize through ads and affiliate marketing. 8. Virtual Second Opinion Consultations: Offer virtual second opinion consultations for patients seeking additional insights on their healthcare decisions. Provide your expertise through video consultations. Ok, I have to be honest, this makes me nervous. Talk about HIPAA and liability concerns. So, if you do this, I’d consult with a lawyer first. 9. Holistic Health Workshops: Host part-time workshops on holistic health practices, such as meditation, mindfulness, or herbal remedies. Charge participants for attending. Such a growing area! 10. Health-related Affiliate Marketing: Promote health and wellness products as an affiliate marketer. You can earn commissions for every sale generated through your referral links. 11. Teach Nursing School Clinicals or be PT Clinical Faculty or Adjunct Faculty: Whether it’s LPN, RN, BSN, MSN, or DNP, there is a shortage of faculty for nursing programs. My colleague did 2 classes a year for several years at a State University, and now she has qualified for a pension! 12. Chart Reviews for Attorneys: Many seasoned NPs love this little side gig! 11. Precepting: Educating the Next Generation of NPs and PAs! You know we love this one! Mentoring aspiring NPs and PAs as a clinical preceptor is not only a fulfilling side hustle but also a way to give back to the profession. By sharing their expertise and experiences, NPs and PAs play a vital role in shaping the future of healthcare by educating and guiding the next generation of Nurse Practitioners and Physician Assistants. (Explore more through www.PreceptorLink.com, where we can offer an honorarium for preceptors.) In the world of healthcare, Nurse Practitioners and Physician Assistants are not limited to their primary roles. Side hustles allow NPs and PAs to diversify their careers, impact their communities in new ways, and enhance their financial well-being. Whether it's through telehealth consultations, wellness coaching, medical writing, consulting, or preceptorship, NPs and PAs can harness their skills and passion to unlock a world of opportunities. Tell us what you have done and what your experience was like. And tell us about other side hustles we might not have listed! Lillie’s story is one of resilience and unwavering dedication.
An experienced Certified Nurse Assistant from Cameroon, Lillie harbored the dream of advancing her nursing career in the United States. Her journey was arduous, yet driven by passion, she moved to the States and earned her Associate of Science in Nursing in 2019. Despite the challenges of meeting the stringent requirements to become an RN in the U.S., Lillie persevered. I had the pleasure of assisting her in securing a pediatric preceptorship to complete her final 40 hours—a step that would finally crown her efforts. Today, Lillie is not only an RN but also a beloved figure among her patients, who commend her as "the best nurse on the unit." Now, she sets her sights on a Bachelor of Science in Nursing, continuing to inspire and aspire. Lillie's success story shines a light on the potential solution to the nursing shortage plaguing the U.S. healthcare system. The shortfall, fueling burnout and high turnover, calls for innovative resolutions, one of which is embracing the contributions of international nurses like Lillie. These professionals often bring diverse experience and new perspectives to patient care, yet they face considerable barriers to practice in the U.S. Streamlining the transition for these international nurses is a promising avenue for addressing our healthcare needs. The process, involving credential recognition and cultural acclimatization, demands both compassion and efficiency. We must uphold the high standards of care while easing the integration of these qualified individuals into our medical community. Supporting international nurses in their journey doesn't detract from the necessity to tackle core issues such as burnout and educational constraints. However, their inclusion can provide temporary relief and enrich our healthcare tapestry. As Lillie's story illustrates, international nurses are ready and eager to serve; we must be equally ready to welcome their dedication and skills. By fostering an environment that aids international nurses in realizing their dreams, as we did for Lillie, we do not just fill vacancies. We reinforce a culture of diversity, quality, and compassion that is the hallmark of our healthcare system. Lillie and many like her are not merely filling a gap; they are bringing a fresh zeal to the noble vocation of nursing, reminding us that at the heart of healthcare is the universal language of human care and connection. Lillie's narrative embodies the journey and potential impact of international nurses in the U.S., highlighting a personal story while underscoring the broader implications for healthcare policy and practice. At PreceptorLink® we could not be more happy and proud to help amazing colleagues like Lillie accomplish their dreams! Congratulations, RN Lillie! Are you tired of being a kind and nurturing preceptor? Are you looking for new ways to make your students' lives just a tad more challenging? Well, you're in luck! Here, we'll explore some unconventional and humorous strategies to keep those eager students guessing and occasionally questioning their career choices. (This is the counter of my last article, “The Art of Annoying Your Preceptor: A Masterclass in What Not To Do." It seemed only fair to play both sides of this!) Remember, this is written tongue-in-cheek, and we certainly are NOT making light of these real situations that students report. As always, we encourage positive teaching practices and quality education. Let's dive into the world of “Preceptor What Not To Do’s.”
1. The Art of Misleading Guidance Why give clear and concise instructions when you can leave your students utterly baffled? Offer cryptic guidance, like "You'll know it when you see it" or "Trust your instincts." Watch as they struggle to decode your enigmatic wisdom. (Although this can be true!) 2. The Rotating Expectation Wheel Keep your students on their toes by frequently changing your expectations. One day, emphasize the importance of a complete history when reporting; the next, act as if it's an optional concept and tell them you don’t have time for all this information. This rollercoaster of expectations will leave them exhilarated (and confused). 3. The "Withholding Information" Game Why spoon-feed knowledge when you can make your students work for it? Deliberately withhold essential details and watch as they embark on wild goose chases for information they didn't know they needed. 4. The Mystery Diagnosis Challenge Create a medical mystery that Sherlock Holmes himself would struggle to solve. Give your students obscure symptoms and contradictory test results. Bonus points for making them question their medical knowledge. 5. The Rapid-Fire Question Round During rounds or presentations, fire a relentless barrage of questions at your students with no regard for their confidence or preparedness. Encourage your colleagues to join in for maximum stress. 6. The "Impending Doom" Vibe Maintain a perpetual aura of impending doom during your teaching sessions. Throw in phrases like "This is a make-or-break moment," "The stakes have never been higher," and "Good luck." Bonus points if you can make them break a sweat. 7. The Accidental "Over-The-Top" Sarcasm Incorporate sarcasm into your feedback and pretend you're utterly amazed by their simplest accomplishments. For example, "Wow, you managed to tie your shoelaces today. Impressive." 8. The "Missing Mentor" Routine Occasionally disappear for extended coffee breaks or long lunches, leaving your students to fend for themselves. It's essential to test their independence, right? 9. The "Unpredictable Availability" Schedule One day, be overly accessible and offer endless guidance. The next, become a ghost, leaving your students frantically searching for answers. It's all part of the adventure! 10. The Guilt-Inducing Hints Drop subtle hints about the competitiveness of the medical field and the astronomical debt they'll accumulate. Make them second-guess every life choice that led them to your preceptorship. 11. The "Disparaging Dialogue" Act For an extra dose of discomfort, publicly criticize your students in front of colleagues, patients, and anyone who'll listen. Nitpick their every move, question their competence, and make them feel like they're perpetually under a microscope. Remember, sarcasm and passive-aggressiveness are your best allies in this endeavor. (Please don’t do this! If you need to speak to your student, do it privately and professionally. If needed, bring in their faculty.) We LOVE and value our preceptors! But, just like students, not all have the most ideal teaching skills. Building a positive and supportive learning environment is the key to producing confident and capable clinicians. So, go forth and do your best at precepting! Consider adding a dash of humor and a whole lot of encouragement! Ah, the age-old quest to find ways to annoy your clinical preceptor - a noble endeavor indeed! While I don't condone such behavior, this is a REAL list of things that preceptors have reported. Granted, most students are not like this. Most are great, but you may see some of these things if you precept enough students! Please avoid these things so you don’t drive your clinical preceptor to the brink of madness.
1. Arrive Fashionably Late. Show up to your clinical rotation 10, 15, or even 30 minutes late every day. After all, who needs punctuality in the medical field? Your preceptor will be thrilled to start their day with the delightful surprise of your tardiness. 2. Dress to Impress... the Wrong Way! Forget about wearing professional attire; opt for something more whimsical. A Hawaiian shirt and flip-flops combo will surely make a memorable impression. Plunging neckline or mini-skirt will be sure to keep patients attentive and cause a stir with the office staff! 3. Question Everything. Never miss an opportunity to question your preceptor's orders, diagnoses, or treatment plans. Make sure to do it loudly and in front of the entire medical team for maximum impact. And don’t forget the eye-roll or dismissive comment. 4. Interrupt, Interrupt, Interrupt. Don't let anyone finish a sentence, especially your preceptor. Jump in with your thoughts, irrelevant anecdotes, or the latest trending meme. Conversation skills are overrated, anyway. 5. Google It All. Why rely on your preceptor's extensive medical knowledge when you have Google at your fingertips? Constantly fact-check them during rounds, citing the first search result you find. 6. Never Take Notes. Who has time for jotting down important information? Just wing it and rely on your photographic memory (if you have one). Your preceptor will be in awe of your abilities… or not. 7. Overshare Personal Details. Ensure your preceptor knows your entire life story, from your pet hamster's dental problems to your Aunt Martha's knitting hobby. They'll appreciate the diversion from actual medical work. 8. Forget About Hygiene. Personal hygiene is for the weak. Show up smelling like a dumpster on a hot summer day, and you'll be unforgettable, albeit not in a good way. 9. Take Really Long Lunch Breaks. Lunchtime is for napping or making TikTok videos, not for discussing cases or learning from your preceptor. Take excessively long lunch breaks. Come back late again. 10. Constantly Complain. Complain about everything - the workload, the hours, the patients, the drive, the coffee in the break room, and the fact that you have to wear pants. Your preceptor will surely admire your positivity. 11. Disdain Their Patient Population. For your peds (or whatever) rotation, mention that you "hate peds and are only doing this rotation to check off the box.” This will really motivate your preceptor to teach you about his/her passion and profession! Okay, we hope this is more funny than truthful to you! Obviously, it's crucial to maintain professionalism and respect when working with clinical preceptors and colleagues. Building a good relationship with your preceptor is essential for your education and future career, so be sure to demonstrate your dedication and commitment in a positive and respectful manner. Who knows, they might provide a good reference or be on the other side of the interview table someday. Stay tuned! Next, we’ll flip this topic on its head and talk about things that Preceptors do that make life particularly hard on students! As the nurse practitioner owner of PreceptorLink®, I've always held a keen interest in the nuances and changes happening in our industry. Owning a business gives you a vantage point to see things not just as an individual, but as part of a broader community. Combining my longtime background as a clinician with the role of a business owner, I have a unique perspective. Today, I'd like to share with you some intriguing insights that I believe will resonate with our entire profession.
Our team at PreceptorLink® values feedback immensely. Every bit of praise, concern, or suggestion helps us recalibrate our efforts to serve you better. A significant part of our mission is to exponentially grow the number of available and willing clinical preceptors for APRNs and NPs. With this aim in mind, we routinely send out surveys to all our clients, assessing their satisfaction with our services and inquiring about their willingness to precept in the future. One pattern has emerged from these surveys that I find both enlightening and somewhat alarming. After reviewing numerous student surveys, we've noticed a direct correlation between their experience with preceptors and their future intent to precept. Specifically, students who expressed dissatisfaction with their preceptor or clinical rotation were considerably less inclined to consider precepting in the future. However, it's crucial to add perspective here. This is not necessarily a reflection of the quality of the preceptors. In over nine years of preceptor matching, we've placed thousands of students, and, while we always strive for the best matches, not every student will have a “great” experience. Many elements can factor into this equation: fit, personalities, schedules, school issues, and communication, just to name a few. It's unrealistic to expect every student-preceptor pairing to be flawless. We've come to appreciate that every story has two sides. Ponder the implications of these findings. If our students of today, who are our potential preceptors of tomorrow, carry negative preceptorship memories, it could significantly impact the availability of future preceptors. This realization underscores the importance of ensuring students are matched with quality preceptors. It's not just about the immediate learning experience; it's about fostering a mentorship cycle crucial for our profession's growth and quality. This observation is not an indictment but an intriguing aside we've witnessed, which the profession might want to explore further. Rest assured, our team doesn't take this lightly. Every piece of feedback, whether positive or negative, is thoroughly reviewed. We believe in looking at both sides of every story. It's not just about addressing student concerns but also about understanding the challenges and viewpoints of preceptors. We can help bridge gaps, mend misunderstandings, and facilitate growth by fostering open communication and creating a balanced environment. In closing, I'd like to reiterate our commitment at PreceptorLink® to creating a nurturing environment for all. The students of today are poised to become the providers, mentors, and leaders of tomorrow. Let's ensure they have the best possible experiences, so they are inspired to give back to the community when the time comes. If we all work together, understanding the intricacies and influences of our actions, we can create a bright future for the NP profession. Thank you for being an integral part of this journey. Your feedback, partnership, and trust are what drive us to do better every day. Education remains the cornerstone of excellence for the ever-evolving world of nursing professionals. Over the past several years, Nurse Practitioner (NP) and Advanced Practice Registered Nursing (APRN) education has been reshaped by the rise of online education. Additionally, online education for APRNs has been reshaped by Online Program Management (OPM) companies. As with all innovations, OPMs have brought both opportunities and a set of unique challenges. Understanding this landscape can be crucial for nursing professionals seeking to upgrade their expertise or enter the field of advanced practice nurse.
The Rise of Online Program Management in NP Education Online Program Management companies have become integral partners for many universities and educational institutions. The goal of an OPM is to help in the design, administration, and delivery of online courses and programs. Traditionally, NP/APRN programs have been bound by geographical limits. However, with the assistance of online education, institutions can now reach aspiring NPs/APRNs from virtually anywhere, thus broadening their student base and increasing accessibility. Pros of OPMs in NP/APRN Education: Expertise and Resources: OPMs bring technological know-how and resources, helping institutions launch sophisticated online platforms that might have been out of reach otherwise. Marketing and Recruitment: With expertise in digital marketing, OPMs can attract a broader student base, enhancing enrollment and diversity. Data Analytics: OPMs often utilize analytics to improve course offerings, tailoring them to students' needs and potentially improving outcomes. Cons of OPM in NP/APRN Education: Quality Concerns: With the rapid proliferation of online programs, there are concerns about maintaining the caliber and rigor, especially with NP education. As OPMs focus on scalability and profitability, there's a concern that the quality of education might be compromised. It's essential to ensure that online courses uphold the same standards expected for any quality NP educational model. Financial Implications: While OPMs can expand a university’s reach, some OPMs operate on revenue-sharing models, which might take a significant portion of tuition fees. This arrangement could potentially inflate tuition costs and raise concerns about online programs' cost and value proposition. Loss of Institutional Autonomy: Partnering with OPMs might mean relinquishing some control over course creation and management, potentially diluting the institution's unique value proposition. This could prove frustrating for faculty and students alike. The entrance of OPMs into the advanced practice nursing arena has amplified both the opportunities and concerns. As highly educated nursing professionals, it's imperative to approach online education critically, recognizing its strengths and limitations while still advocating for standards that uphold the esteemed tradition of the nursing profession. Ensuring the maintenance of rigorous standards, pushing for a blend of online and in-person experiences, and making informed choices about program selection will all play a part in leveraging the best options for the future of NP and APRN education. Dr. Patrice Little, of NP Student, intervews Lynn McComas, the founder of PreceptorLink®, on the vital role preceptorship plays in transforming nurse practitioner students into skilled professionals. She offers actionable strategies for optimizing clinical experiences and emphasizes the significance of treating these rotations as potential career-defining opportunities. Do you remember the good ol' days when Nurse Practitioners (NPs) depended on Dr. Google or Facebook to answer medical queries? Oh wait, we still do! 🥴 But the future is knocking at the door, and its name is AI! Yes, folks, Artificial Intelligence is no longer confined to those creepy sci-fi movies. It’s sneaking into our lecture halls, clinical labs, and even popping up during coffee breaks. I’m a natural-born innovator, so AI doesn’t scare me. It excites me! So, let’s explore how NPs can buddy up with AI without becoming part-time robotic overlords!
1. The "Know-it-all" Virtual Assistant: Ever had that midnight question that keeps you tossing and turning in bed? Instead of pinging your already-overwhelmed NP study group, ask your friendly AI assistant. They're up 24/7, and no, they don't get annoyed by your constant "Why's." 2. No More "Dummy" Patients: Tired of practicing on plastic dummies that neither complain nor compliment? Enter AI-driven virtual patients. They can mimic real-life symptoms, ask confusing questions, and even fake a dramatic fainting episode (all without actually hurting anyone). 3. Study Buddy Extravaganza: AI can track what you're good at and where you're, well, let’s say, "creatively challenged." Personalized quizzes, mock tests, and fun pop quizzes – it's like having a personal tutor without the stern looks and heavy sighs! 4. “You’ve Got Mail! And it’s a Research Update!”: Keeping up with the latest research articles can be as tricky as chasing a toddler with a chocolate bar. AI can sift through those zillion pages and give you a neat little summary, allowing you more time for, well, chasing toddlers (or more studying). 5. Role-playing? Game On! Remember those cringy role-play sessions in class? (Or am I dating myself?) AI's got you covered! Interact with virtual patients, diagnose them, and get real-time feedback. Plus, these virtual folks won't gossip about you in the cafeteria later. 6. Bye-bye Administrative Nightmares: Oh, the joy of scheduling, handling paperwork, and chasing after assignment deadlines. But guess who loves these chores? Our AI pal! Let it handle the boring stuff while you focus on the exciting world of stethoscopes, clinicals, and patient smiles. 7. Ethics Training with a Twist: Imagine a virtual world where you're the superhero NP navigating a maze of ethical challenges. With AI simulations, learn about tricky situations in an environment as fun as a video game (just without the zombies)! So, my NP colleagues, gear up for an AI-filled future where learning is fun, fast, and fabulous! And if you ever feel overwhelmed, just remember – while AI might know the entire medical encyclopedia, it still can't find its way around a band-aid! Cheers to human touch (and occasional goof-ups)! 🤖👩⚕️🎉 Hi everyone, it's Lynn McComas, DNP, ANP-C, the nurse practitioner owner of PreceptorLink®. In this video, I will provide you with tips and suggestions on how to find your own preceptor for your rotations. I will discuss the importance of knowing your school's requirements, creating a well-written cover letter and resume, networking opportunities, affiliations with hospitals, and being persistent in your search. If you want us to take the preceptor search off your shoulders, we are happy to help! Please reach out to us at www.preceptorlink.com. Keep on learning! 00:00 Introduction 00:19 Knowing School Requirements 00:58 Creating a Cover Letter and Resume 02:09 Networking Opportunities 02:33 Joining Professional NP Associations 03:29 Utilizing Facebook Groups 03:53 Affiliations with Hospitals 04:59 Pounding The Pavement 05:52 Be Open To Travelling 07:11 Persistence Pays |
About Lynn:As a longtime NP with a desire to help and make positive changes to her beloved profession, Lynn often writes opinion pieces about the NP profession. Archives
July 2024
Categories
All
"Why NPs train on the backs of physicians"
from KevinMD |
|
Jeremiah 29:11
PreceptorLink, Inc.®️ All rights reserved. Website Design by WCW Designs
|












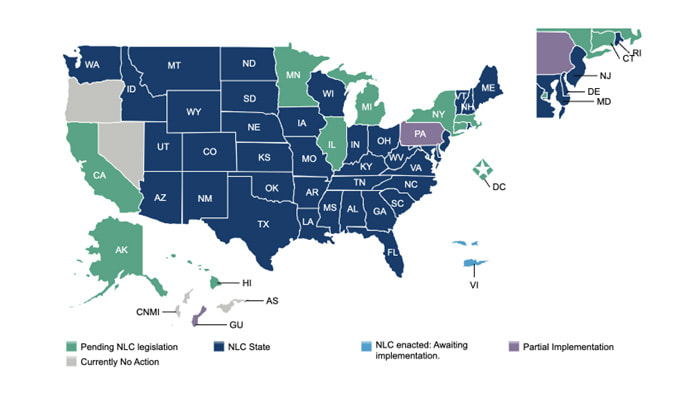







 RSS Feed
RSS Feed

